Our team is dedicated to providing the highest quality care in testicular cancer treatment.
Here are some common questions about our Testicular Cancer treatment and how we can help you.
We provide comprehensive treatment options for testicular cancer, including surgery, chemotherapy, radiation, and advanced immunotherapies, customized to your specific diagnosis.
Yes, we offer fertility preservation services, such as sperm banking, for patients who are concerned about potential effects on fertility due to treatment.
Our recovery services include physical therapy, emotional counseling, follow-up care, and support groups to ensure that patients regain their strength and well-being during the recovery process.
We offer access to the latest clinical trials for testicular cancer patients, providing opportunities to receive cutting-edge treatments and therapies that may not be widely available yet.

Each patient’s journey is unique; we tailor treatment to your specific needs.

Work with top cancer specialists focused exclusively on testicular cancer.

Receive counseling and support during your treatment process to help manage stress.

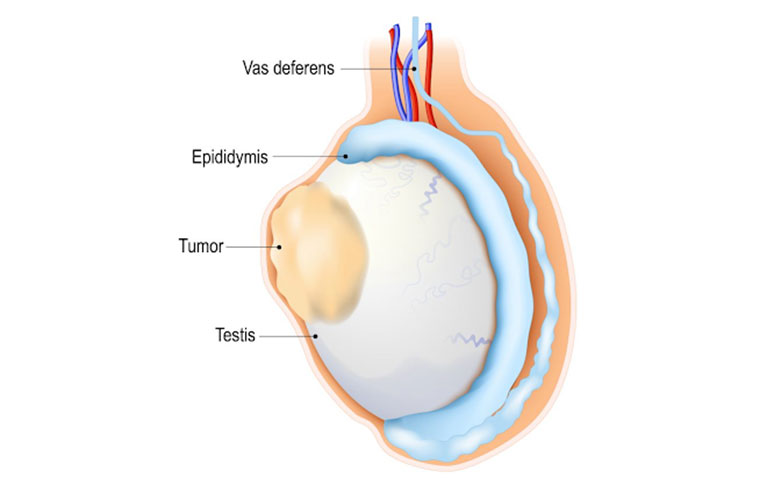
Get accurate and timely diagnostics for effective treatment decision-making.

Explore our Tie ups for Cashless insurance and Income tax exemption services.

Our care extends beyond immediate treatment to focus on fertility and child bearing potential post-treatment.
Deciding on cancer treatment can be intimidating, but our specialists are here to address your fears and provide reassurance.
We offer various financial options and will work with you to discuss treatment financing.
Our team ensures to inform you about potential side effects and works to manage them effectively.
You are not alone; we provide supportive resources that help you cope with stigma and anxiety.
We use evidence-based treatment methods personalized to your unique diagnosis to achieve the best outcomes.
Our pricing structure is transparent and competitive, ensuring patients receive premium care within their budget.
Detailed evaluation and discussion of symptoms.
Prices vary based on tests required.
Costs depend on the type of treatment selected.
I felt cared for every step of the way.
Hear from our patients about their experiences.